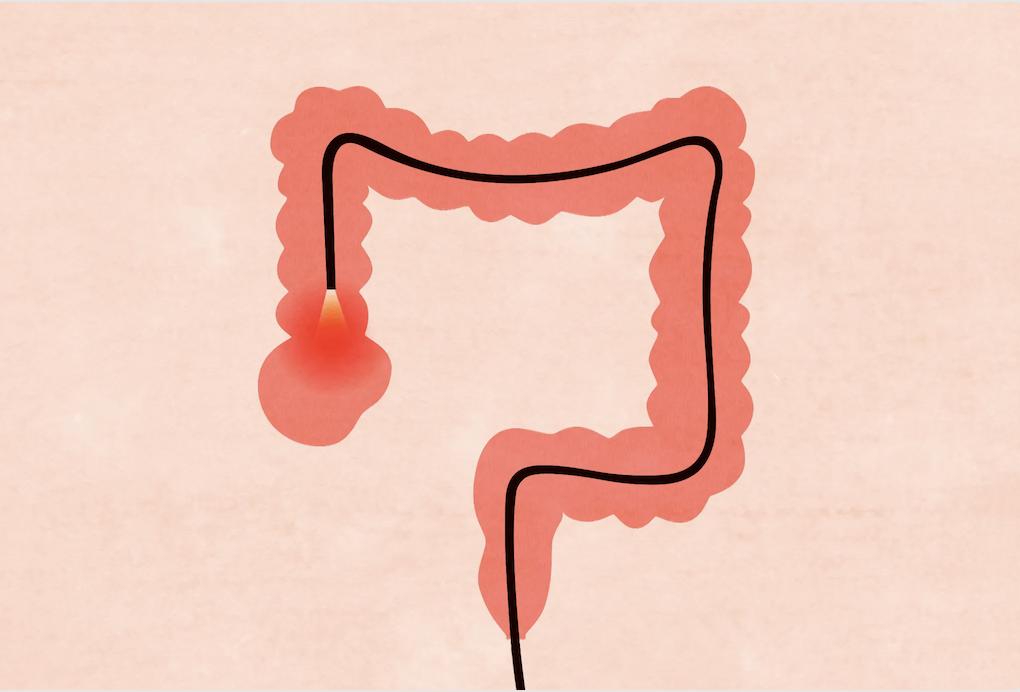
I’m a person who has a mammogram once a year. As part of routine preventative health care, I also have a colonoscopy procedure in accordance with the national standards for frequency. Although only 8% of newly diagnosed cancers are colon cancers, early detection and treatment dramatically reduces death rates. So colonoscopies are very valuable and I would want to continue to have them as recommended.
What I have discovered is while the procedure itself may have minimal complications, the anesthesia used may put patients at unnecessary risk for aspiration pneumonia. While I have since learned of two individuals in Easton who developed aspiration pneumonia after their colonoscopies, my own complication was nodules on my vocal cords and laryngitis because of severe coughing as I came out of the anesthesia. Not being able to speak was finally alleviated after six months of steroid injections in my vocal cords (extremely unpleasant) and voice therapy at Johns Hopkins.
It was only when I investigated what had happened to me that I learned I was lucky. The documented most frequent complication from colonoscopy with deep sedation is not damage from the colonoscopy procedure itself but the aspiration pneumonia resulting from the anesthesia. And not just any anesthesia but deep sedation that is in recent vogue at endoscopy centers since it’s possible to do more procedures in a day than with the previously popular but less risky moderate sedation. (Cooper et al, JAMA Internal Med/vol 173:7. Apr 8, 2013)
What’s the big deal about deep sedation vs. moderate sedation?
Moderate sedation makes you drowsy cognitively but the protective reflexes in your throat which allow you to clear your throat and cough to protect your lungs from inhaling stomach acid etc. continue to function. With deep sedation those reflexes do not function during at least 20 minutes while you are lying flat on your side so that when you wake up you are at risk of coughing severely to clear your throat of what has accumulated there (like me) or much worse than that, your coughing is unsuccessful and you aspirate acid or other stomach contents into your lungs leading to aspiration pneumonia.
What to do? Before your colonoscopy talk to your Gastroenterologist about the anesthesia you require and make sure the endoscopy center is prepared to provide that when you make your appointment.
This is a cautionary tale as someone who didn’t go through a Gastroenterologist and didn’t have the anesthesia options explained as the anesthesia provider was required to do.
Holly Wright
Easton

Darrell parsons says
Thank you, Holly.
Carol Crutchfield says
Thanks Holly.
Michael J. Fisher, M.D. (Retired Gastroenterologist) says
This is a response to Ms. Holly Wright, who recently wrote of her unfortunate experience of colonoscopy. I have spent my entire career watching the evolution of cancer prevention strategies, and even though this vital exam has it’s risks and discomfort, it works. We see the flags waving for Colors of Cancer in our streets and along the bypass. It remains, despite the advertising for noninvasive stool tests, the best strategy for diagnosing colon cancer and treating lesions likely to become cancer. Colon cancer mortality has fallen over the past decades, coincident with higher numbers of the eligible population being screened, until COVID, when people deferred their exams or clinics were closed to elective procedures. In selecting patients for outpatient procedures, risks are assessed, depending on age, pre-existing disease states, and special needs based on the individual, and if any increased risk is identified at any time, even in a prepped patient, the procedure is cancelled. Some patients require being done in hospital, which entails a much greater cost and overwhelms the already-stressed medical system. When I was in practice, our outpatient endoscopy clinic formerly used medicines like Fentanyl and midazolam. However, they were associated with prolonged sedation, hypotension, hypoxemia, vomiting and yes, even the rare aspiration pneumonia too. I have had these medicines myself, and in addition they caused hours of amnesia. This approach also reduced the numbers of patients who could be screened, because they take much longer to recover. Propofol, administered by licensed anesthesia providers, allows for rapid recovery of those protective reflexes. For the endoscopist, it allows for deeper and more complete examinations, higher polyp detection rates, patient satisfaction rates (Clin Exp Gastroenterology 2019: 12:105-110), plus less patient movement during the procedures, which is otherwise is exhausting physically. It allows for greater concentration on the exam itself and less on the drug administration. These advantages being said, they do come with concerns and risks, because the level of sedation during the procedure is greater. The prep for the procedure itself is not pleasant, and in some regimens high volumes of liquid are used to clean the bowel, which can be retained in the stomach at the start of the procedure and subsequently vomited. Protocols are used by every certified endoscopy clinic to reduce complications, and doctors who perform these procedures spend years of training so that safe outcomes can be obtained. Complications are reviewed and discussed at Quality Review committees.
No doctor or clinic is perfect, even though our society would believe this is so. It’s easy to become cynical about the business side of medicine, too. But as a doctor, it is a difficult thing to get through when we have a complication, believe me. And we all have had those complications, despite our best intent. I have been a patient, lying on a stretcher being wheeled into the operating suite, knowing this. There is an oath we take as physicians– “To Do No Harm”, and no doctor I have known is glib about complications. We have risks if we get in our car, drive on the Beltway, have babies or fly on a plane, but we do it. Cancer can be prevented, and right now, colonoscopy is not only the best way to achieve this in 2022, but precancerous lesions can be eliminated. We each have about a 1 in 20 chance in our lifetimes of getting colon cancer, the number 2 overall cancer killer in our country. I chafe at the reference to “Colonoscopy Mill”, and I am sorry she feels this is so, but I truly appreciate the discomfort she has suffered. And I agree with her that, given anesthesia or any other health concerns, it is a reminder for providers and patients to have a dialogue before any medical procedure is undertaken. But anything to dissuade people in our community to have this lifesaving procedure is unhelpful and risky in a different sense. Thank you.
Holly Wright says
Thanks, Michael. I read with interest the study you cited. (The internet is great for making journal articles accessible.) The complications that were considered in relation to deep sedation vs moderate sedation were cardiovascular (hypoxemia, hypotension, and arrythmias) and did not include aspiration or aspiration pneumonia which is a known complication of deep sedation.
Anyway, as I was careful to say at the outset, a colonoscopy is a valuable part of preventative health care and as you say, life-saving. At the same time, there are risks associated with various options for anesthesia which we agree should be discussed with the patient ahead of time. My suggestion is that that conversation is better had with a Gastroenterologist before the day of the procedure and not to rely on the anesthesia provider at the endoscopy center on the day of.
Michael K Henry says
I read with interest the letters on the subject of colonoscopies and endoscopies. I have had both because of being diagnosed twice with colon cancer. I have Barrett cells hence the endoscopy.
Most recently I had these tests March of 2022.
I was told by my urologist that these tests were not done routinely on elderly patients. I am eighty and think that I would qualify. My primary medical person dismissed this and these test were arranged. No side effects were ever mentioned.
Fortunately both tests were negative for cancer.
Later that day I felt uncomfortable and then in pain. I went to the emergency room and a catheter was installed.
That situation remains the same. I am unable to urinate on my own and have had to wear a catheter all the time including the night time.
I have had tests regarding my situation but so far nothing has helped. I am beginning to think that I might be stuck with this problem for life.
I write this letter not to denigrate the usefulness of these procedures but I do think that patients should be made aware of possible slide effects.
I have done a little research of my own and although unusual my problem is not unknown.